Author: Bram Kuiper
In 1985, just one year after being diagnosed with pancreatic cancer, my father passed away, aged 63. As a doctor he knew right from the diagnosis that he wouldn’t survive. My mother, two sisters, two brothers and I surrounded him with all the attention, love and support he needed. My father always kept a diary and in one of his entries he wrote that his illness felt like a stay in a foreign country. He was familiar with that feeling because he spent many years abroad working as a doctor in the tropics. I was 29 years old and working as a clinical psychologist. It was my first serious experience with cancer and for me it also felt like spending time in a foreign world. But during that year, it became more and more familiar, no matter how bleak the future seemed to be.

Two years later, in 1987, I started as a psychologist at the Free University Medical Centre in Amsterdam. That I would include working at the Oncology Department alongside my other tasks was self-explanatory. I provided care for cancer patients, their family and friends, with different types of cancer, young and old, with good and bad prognoses, both inside the clinic as well as in the outpatient clinic. It all felt very familiar. Later, in 2000, I became CEO of the Helen Dowling Institute, a fabulous and renowned psycho-oncology centre in the Netherlands. Until 2012 I combined my job as CEO with my work as a psychologist.
Over the last 30 years I have witnessed the enormous impact cancer has on the physical, emotional and social life of patients and their loved ones from different perspectives: as the child-of, the brother, the partner, the friend, the colleague and the psychologist. What have I learned?
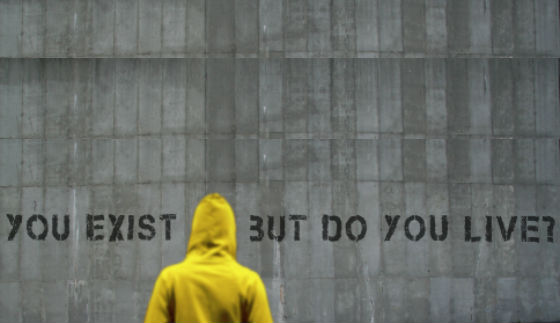
I have come to realise that the essence of oncology revolves around the issue of ‘to be’ or ‘not to be’. This applies both literally and figuratively, for everyone dealing with cancer.
First, it applies to people who have been diagnosed with cancer. Sooner or later they will ask themselves ‘How long do I have to live? How long will I be here?’ Literally, ‘to be’, to live, because ‘not to be’ implies the end, death. It’s all about the quantity of life. Even when the prognosis is ‘reasonable’ to ‘good’. And when you still have time to live, however short that may be, sooner or later a second question presents itself – about the quality of life. ‘How do I want to live? How do I want ‘to be’ as long as I’m still here?’ ‘What do I still want (or do not want) to do’, that’s what it’s all about. Once they are confronted with cancer, people re-evaluate their desires and limitations. Figuratively, ‘not to be’ implies the absence of quality of life. People with cancer want ‘to be’, both literally and figuratively.
Second, it applies to everyone who works in oncology. ‘To be’, or ‘not to be’. Literally it means one should physically be present enough and also offer the best possible care. That’s the least you can do. At the same time you need to be present figuratively, by which I mean that caregivers should be ‘attentively available’ for patients trusted in their care. People with cancer go through an existential crisis and in my opinion they sense immediately when someone isn’t truly involved – whether they ‘are there’ or ‘not there’.
Only when caregivers are truly ‘there’ they can genuinely help their patients ‘to be’ in the strange unknown country. Literally and figuratively


 Everybody gets tired at one time or another. Cancer-related fatigue, however, is not ‘normal’ fatigue. It’s mental and physical exhaustion. It has a huge impact on every aspect of your life. It can kick in totally unexpected and rest or sleep doesn’t help to get your energy back. You may wake up in the morning, drag yourself to the shower, undress and… you’re exhausted again. This is a pretty common example of the severe fatigue you may be experiencing. CRF is different for different people though. If you feel in any way that you are abnormally tired or lack energy, talk to you doctor about it.
Everybody gets tired at one time or another. Cancer-related fatigue, however, is not ‘normal’ fatigue. It’s mental and physical exhaustion. It has a huge impact on every aspect of your life. It can kick in totally unexpected and rest or sleep doesn’t help to get your energy back. You may wake up in the morning, drag yourself to the shower, undress and… you’re exhausted again. This is a pretty common example of the severe fatigue you may be experiencing. CRF is different for different people though. If you feel in any way that you are abnormally tired or lack energy, talk to you doctor about it.